Playbook
Depending on a doctor's decision, patients with a serious eye condition can be treated successfully with one of two equivalent drugs from the same manufacturer-yet one treatment costs 13 times more. The difference depends on whether the doctor prescribes the less expensive, off-label version.
For the eye condition known as wet AMD. off-label Avastin is just as effective as FDA-approved Lucentis, and much cheaper. Numerous market factors and obstacles explain why high-priced versions persist. This case study traces the path to market of Lucentis and Avastin to explore the many factors that influence the cost and accessibility of an important drug.
What is "Off-label" Usage?
When a drug approved to treat one condition is used by doctors on a different condition for which that drug is not specifically approved, that is “off-label” use. [4] This practice is permitted by the FDA and is commonly used. [5] Health care providers weigh a host of factors to decide what to prescribe, while cost could be an important part of the discussion, often it isn’t.
Imagine you are prescribing a drug for wet AMD. Which would you choose?
From Production to Patient
Two equally effective drugs came to market at different prices and underlying incentives and obstacles contribute to the use of higher-cost Lucentis when a comparable lower-cost option is available.
Learn about the key factors in production that influence a drug's price:
Research & Development
Genentech Sticks with Lucentis Over Avastin
Drugmaker Genentech developed and received FDA approval for Lucentis to treat wet AMD. Genentech also developed Avastin to treat colon cancer.[6] Despite learning early on that Avastin may show promise against wet AMD, Genentech never formally submitted Avastin to the FDA for formal approval, leaving it up to ophthalmologists and researchers to recognize the similarity and benefit of switching to off-label Avastin.
Research & Development
Little Incentive to Develop an “Off-Label” Drug
Why didn’t Genentech pursue FDA approval for Avastin? Genentech had little incentive to pursue FDA approval. Given the resources that go into developing a new drug, it’s reasonable to assume Genentech was heavily invested in the continued success of higher-priced Lucentis.[7] Additionally, there may have been regulatory and market forces encouraging Genentech’s position. Lucentis had FDA approval, which meant it could be marketed as having passed the highest standard of evidence for its use. The unique dynamics of the coverage and reimbursement systems in the U.S. meant the drug would find a large market.
Labeling
Research Comparing Off-Label to On-Label Drugs is Rare
Before prescribing any drug off-label, doctors review the evidence to assess effectiveness. Yet comparative effectiveness research in the U.S. is rarely conducted, and when it is, statute limits the ways in which payers, including Medicare, can use that research in making coverage decisions.[8] But one of the most influential comparative effectiveness studies ever conducted in the U.S. found that these two treatments have equivalent effects on visual acuity improvements when prescribed on the same schedule, without marked differences in adverse clinical events.[9]
Reimbursement
Higher-Cost Drugs Net Bigger Payments
In most cases, Medicare pays providers directly and physicians receive 106% of the average sale price for Medicare Part B drugs. This means higher-cost drugs generate more revenue. Other factors also influence doctors’ decisions, including training, clinical preference, academic literature, and the marketing efforts of drug companies. Clinicians ultimately must balance all of these elements and prescribe the drug they feel is best suited to treat their patients.[10] Given the alignment between a higher reimbursement potential and FDA approval, it is not surprising many doctors prefer Lucentis.
Market Share
Avastin Has Less than Half the wet AMD Market
Distribution
Financial Impact is Evident
At present, Lucentis costs Medicare approximately 13 times more per year.[14] The higher price of FDA-approved drugs to treat wet AMD reverberates through the healthcare system, costing patients and taxpayers millions of dollars. This limits the ability of the health care system to leverage Avastin’s substantially lower price.
Distribution
Encouraging Doctors to Switch
What might influence doctors to prescribe Avastin? One scenario would be participation in risk-bearing payment models where payments are capped or tied to the use of highly effective but less costly therapies.[15] Research shows that if Medicare increased the reimbursement amount for Avastin it could increase usage and save patients millions in copayments, thus expanding access.[16]
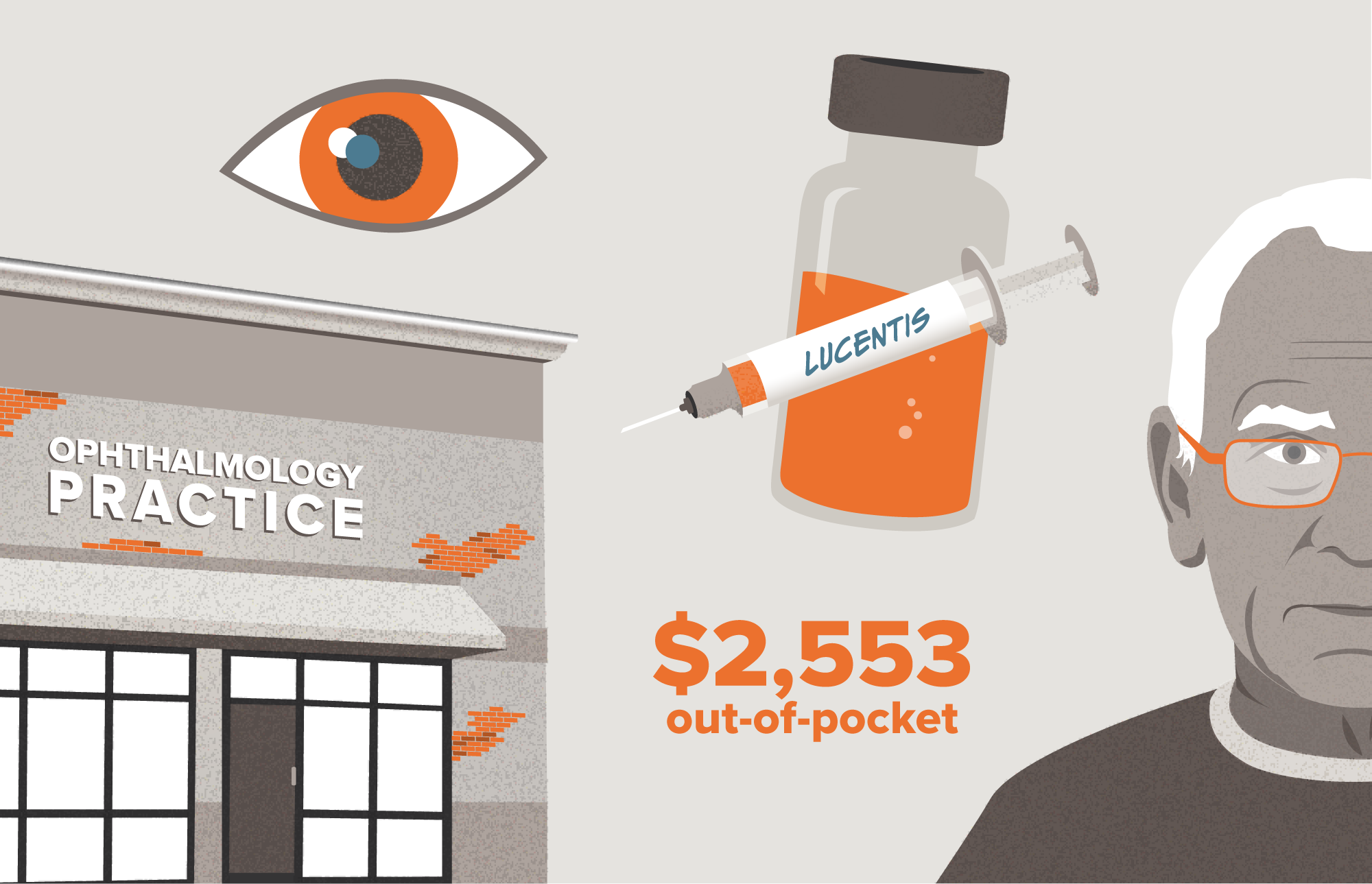
Imagining the Patient Experience
In this hypothetical situation involving a 72-year-old male patient, we see why two medical practices prescribed equivalent treatments, yet one cost the patient more than $2,500 and the other only $361. The price tag is largely shaped by the prescribing provider’s reimbursement structure and incentives.
See how the same patient in two scenarios can end up with very different costs.
Note: Patient scenarios are meant to be illustrative only. Prices are based on publicly available information when available and good-faith estimates when prices were not available.
Off-Label AMD Treatment Fails to Significantly Impact Costs
Two options are equally effective to treat wet AMD. Yet the availability of Avastin, the lower-cost alternative, hasn’t significantly impacted the price of Lucentis, nor has it diminished demand. Why?
One Company Owns Both Drugs
The unique scenario of Avastin, the off-label treatment, produced by the same manufacturer as Lucentis creates an advantage for Genentech.
Reimbursement System Influences Doctors
Payment incentives embedded within the health care system reimburse providers at higher rates when more expensive drugs are administered.